Knee Replacement
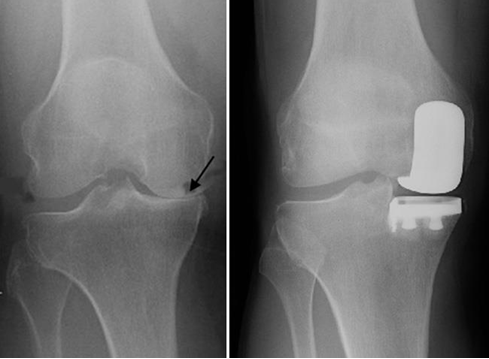
Knee replacement is a surgical treatment for pain caused by knee osteoarthritis or wear. When other treatments have failed to control this pain, knee replacement can be considered. During the operation, the worn joint surfaces are removed and the knee is resurfaced with modern implants.
Why have a Knee Replacement?
The main goals of knee joint replacement are relief of unrelenting pain, to improve quality of life and allow return to normal function (e.g., walking, cooking, sleeping, driving, working).
You may be offered a knee replacement to treat your osteoarthritis but the decision to have the operation is yours. Satisfaction rates from knee replacement are traditionally around 80% (can be as high as 94% with custom knee replacement) and all operations carry some risks. It is sensible to proceed when the anticipated benefits are judged to outweigh those risks.