Hip Replacement
Hip replacement surgery is an operation to treat hip pain. It is a major operation but one that’s both common and successful.
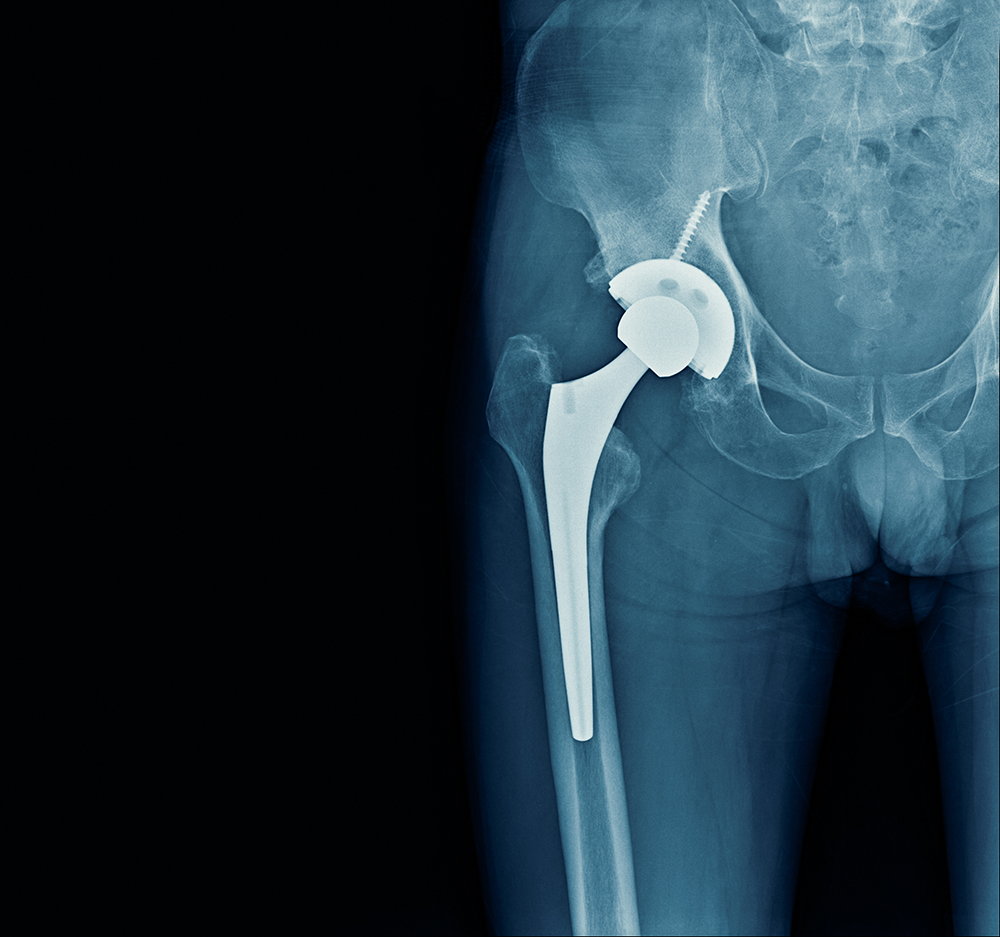
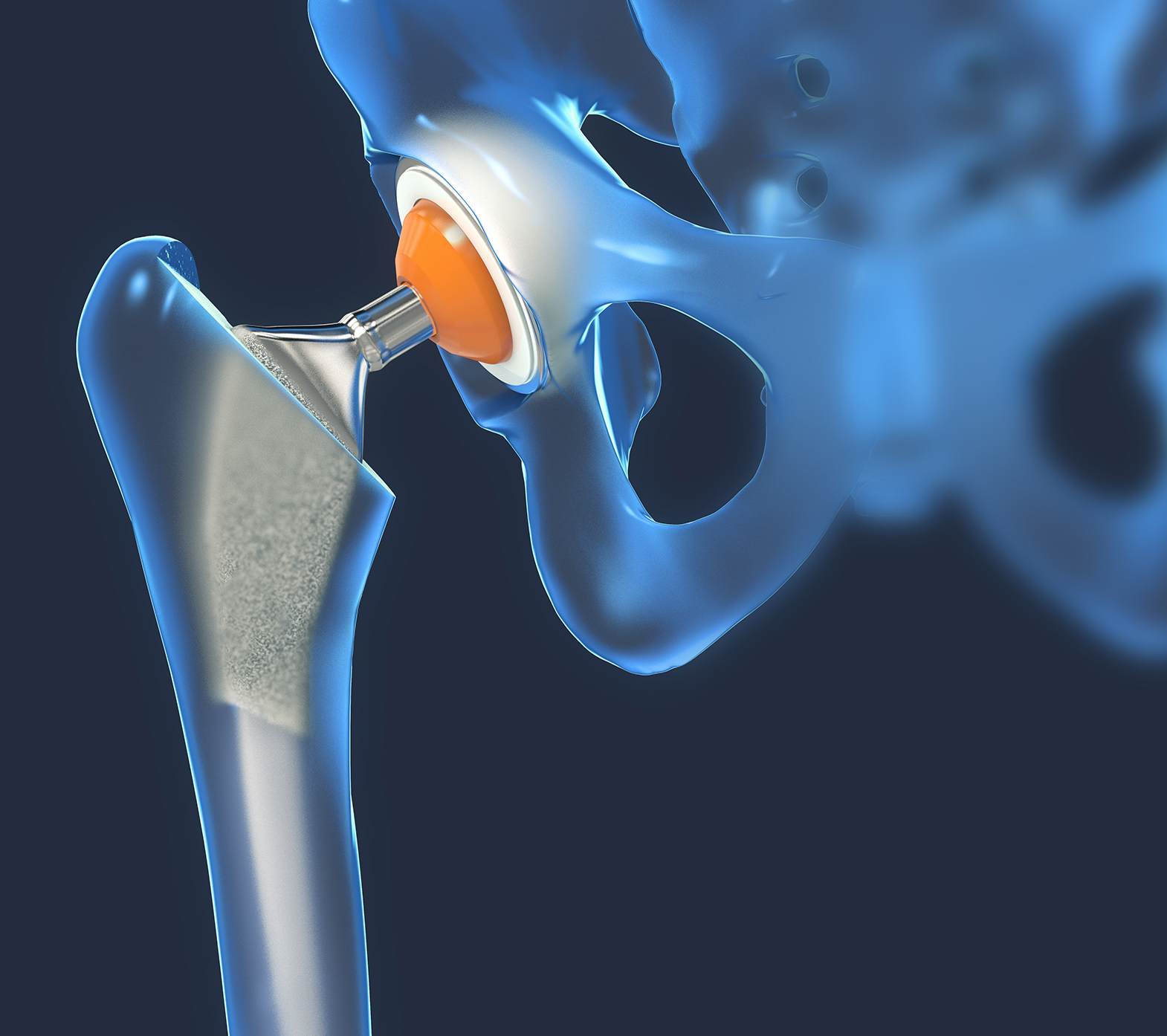
During the procedure, an orthopaedic surgeon will remove your damaged hip joint and replace it with a prosthesis. This is sometimes referred to as an implant or as an artificial hip. The prosthesis is usually constructed of metal, ceramic, plastic, or a combination of the three.
If you are living with a painful hip joint that’s affecting your quality of life, you’ve landed in the right place. Hip replacement surgery could be the best treatment option to help you take control of your health and get you back on your feet, doing the things you love.
This page explains everything you need to know about hip replacement surgery, including information on hip replacement recovery timelines and the benefits of physiotherapy after surgery.